Lesson Progress
0% Complete
Goals of therapy for CMVI:
- Prevent the progression to congestive heart failure in dogs in the preclinical stage of CMVI.
- Only ACE inhibitors have been assessed with respect to delaying the progression of CMVI to the congestive state. In two clinical trials, this class of drug failed to delay the progression of CMVI (SVEP and VETPROOF Trials – see Veterinary Clinical Heart Failure Trials in General Therapeutic Concepts section).
- No other drug or class of drug has been assessed to address this question.
- Data from experimentally-induced CMVI suggests:
- ACE inhibitors may exacerbate the progression of preclinical CMVI
- Beta blockers may delay the progression of preclinical CMVI. More clinical data is needed to know whether, when, and how to use beta blockers in this disease, however their potential appears promising.
- Reduce the amount of mitral valve regurgitation:
- Reduce the regurgitant orifice
- Repair the mitral apparatus
- Not readily available in veterinary medicine yet
- Treatment of choice in people
- Reduce the size of the left ventricle and thereby shrink the size of the mitral annulus
- Preload reduction
- Increase contractility
- Reduce afterload
- Repair the mitral apparatus
- Reduce the driving pressure that promotes regurgitation
- This is accomplished by reducing the difference in pressure between the left atrium and left ventricle
- Reducing the systemic vascular resistance will reduce left ventricular pressure and therefore the difference in pressure between the left atrium and left ventricle
- Afterload reducers (arterial vasodilators)
- Reducing the systemic vascular resistance will reduce left ventricular pressure and therefore the difference in pressure between the left atrium and left ventricle
- This is accomplished by reducing the difference in pressure between the left atrium and left ventricle
- Reduce the regurgitant orifice
- Reduce left bronchial compression by reducing left atrial enlargement.
- Arterial vasodilators may reduce the volume of blood regurgitating across the mitral valve and encourage more blood to move out across the aortic valve. With less blood regurgitating across the mitral valve, the left atrium will shrink somewhat and thus reduce left main bronchial compression.
- Positive inotropes such as pimobendan, at least theoretically, will shrink the annulus of the mitral valve and thereby reduce the amount of regurgitation. This will then reduce left atrial size and hence the amount of compression.
- The irritation that is encountered by the bronchial tree induces secondary spasm.
- Bronchodilators may help relieve this problem.
- Antitussives can help break the viscous cycle of cough-induced coughing.
- If heart failure is present then therapy should include:
- Begin with:
- Furosemide: use the least amount necessary to maintain ease of respiration
- ACE inhibition
- Pimobendan
- Low sodium diet and exercise restriction
- If the patient remains in CHF or becomes refractory to treatment:
- Consider increasing the furosemide dose (as long as renal parameters are normal)
- Consider adding a more potent arterial vasodilator (amlodipine or hydralazine)
- We find amlodipine rather ineffective to reduce blood pressure in this setting. Hydralazine is very effective to reduce blood pressure in CMVI.
- Consider increasing the dose of pimobendan
- Consider adding another diuretic such as a thiazide, if the patient is refractory to high doses of furosemide (and reduce the furosemide dose by half in this case)
- Consider adding spironolactone (but recognize that it is a relatively weak diuretic given its site of action)
- As mentioned above, beta blockers may have a role to play in the treatment of this disease. However more clinical data is needed to know whether, when, and how to use this class of drugs in CMVI.
- Digoxin, in the presence of a sinus rhythm, remains questionable in terms of benefit
- Supraventricular arrhythmias should be treated as outlined in the Supraventricular Tachycardia section of Electrocardiography
- Atrial fibrillation should be treated as outlined in the Atrial Fibrillation section of Electrocardiography
- Acute exacerbation with severe pulmonary edema due to rupture of a chordae is treated as outlined in the Fulminant Pulmonary Edema section of General Therapeutics
- Pulmonary hypertension if present should be addressed. The most promising arterial vasodilator for pulmonary hypertension is sildenafil (phosphodiesterase V inhibitor), however pimobendan may also be useful in this condition
- While sildenafil may improve quality of life for patients with pulmonary hypertension it appears that pulmonary artery pressure does not decrease significantly (Kellum et al. JVIM 2007;21:1258-1264)
- Furosemide – 2-4 mg/kg BID – TID (PO)
- Pimobendan – 0.25 mg/kg BID (on an empty stomach) (PO)
- Amlodipine – 0.1 mg/kg SID (PO)
- Hydralazine – 0.5-2 mg/kg BID (PO)
- Benazepril – 0.5 mg/kg SID to BID (PO)
- Enalapril – 0.5 mg/kg SID to BID (PO)
- Hydrochlorothiazide – 1-2 mg/kg BID (PO)
- Theo-Dur (long acting theophylline) – 20 mg/kg BID (PO)
- Hycodan – 0.22 mg/kg SID-QID (PO)
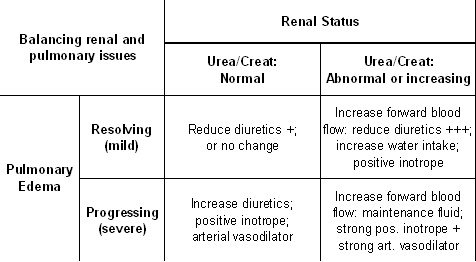
- Sildenafil – 0.5-2 mg/kg BID (PO)Management of congestive heart failure involves controlling vascular volume by finding a balance between meeting renal blood flow needs through enhancing vascular volume (preload) and reducing pulmonary edema by reducing vascular volume (preload).
- Begin with: