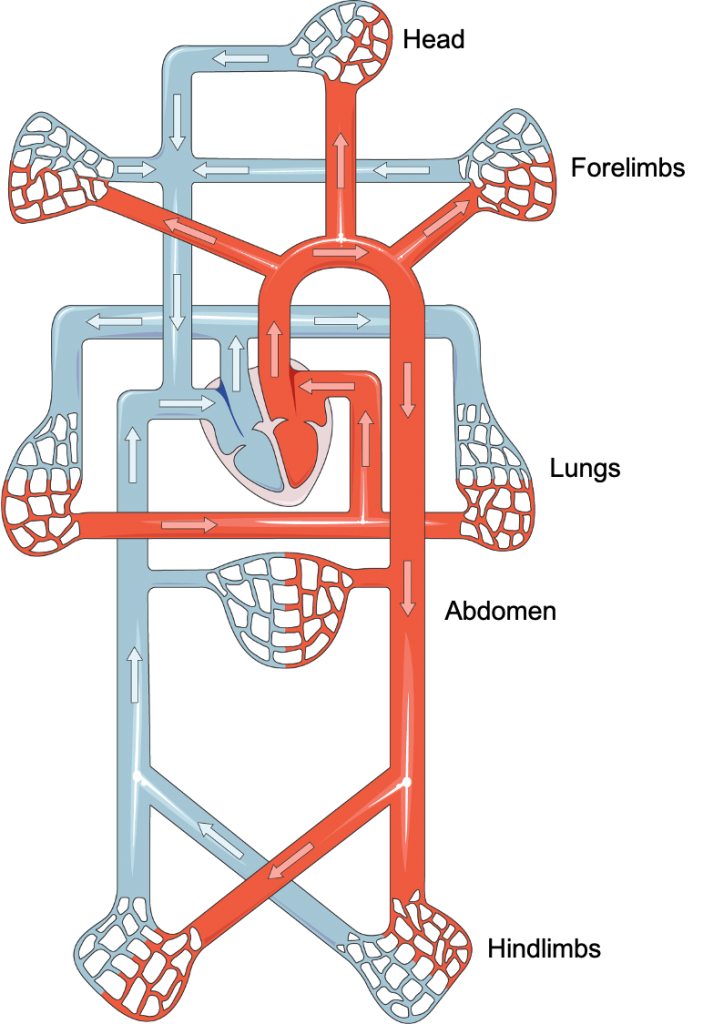
The heart and circulation work together as a pump and a series of conduits and capillary beds to provide oxygen and nutrients to all organs, to provide a means to remove the effluents of metabolism from these same organs, to circulate hormones, and to serve particular organ functions.
Role of the heart
As a muscular pump, the heart is required to eject into the circulatory system a volume of blood appropriate for the metabolic activity and function of the organs. See the next topic (Function of Heart Components) for more.
Role of the systemic arterial system
The large arteries, particularly the aorta, are large conducting vessels:
- They serve to transport blood under high pressure to the organs and periphery
- The elastic properties of the vessel wall promote flow through the periphery during diastole as well as systole
The small arteries are the resistance vessels:
- Relative to the size of the lumen of these vessels, they possess an abundant amount of smooth muscle
- They control blood pressure via the degree of contraction of their smooth muscle in the vessel wall
- They control the steady delivery of blood to the capillary beds
- The arterioles are the last small branches of the arterial system before the capillary beds, controlling the release of blood into the capillaries and having the ability to dramatically alter blood flow in each tissue by contraction or relaxation of smooth muscle
Role of the systemic venous system
The veins are conduit vessels for the return of blood to the heart. They also serve a large reservoir function, holding ~ 70% of the blood volume. Despite being a low pressure system, systemic veins also contain adequate smooth muscle for altering vascular tone. Contraction of the smooth muscle in the venous circulation increases blood return to the heart. Venodilation reduces the return of blood to the heart.
Role of the pulmonary arterial system
The pulmonary arterial system receives the output from the right heart, deoxygenated blood, and delivers it to the lungs for carbon dioxide removal and oxygen loading of blood.
Role of the pulmonary venous system
The pulmonary venous tree collects blood from the pulmonary capillary beds and returns the oxygenated blood to the left heart for delivery to the rest of the body.
Differences between pulmonary vs systemic circulation
The pulmonary arteries, unlike the other arteries of the body, carry deoxygenated blood. The pulmonary veins, unlike the other veins of the body, carry oxygenated blood. The pulmonary arteries respond to hypoxia with contraction, whereas the systemic arteries respond to hypoxia with vasodilation.
Under normal conditions, the right ventricle ejects the same volume of blood that the left ventricle ejects. The pulmonary arterial system is a low-pressure system, unlike the high pressures encountered in the systemic arterial system. The pulmonary arterial walls contain less smooth muscle than the systemic arteries. The reduced amount of tone that can be generated in the pulmonary arterial system is responsible for the lower pressures in the pulmonary arterial system. This arterial tone is also known as arterial resistance. Hence the pulmonary arterial resistance is much less than the systemic arterial resistance.
Role of the capillaries
The function of the capillaries is to allow exchange of gases, nutrients, hormones, and waste products between the tissues and circulation. They are thin-walled and contain pores allowing them to be permeable to select substances.
Starling Forces
Starling forces are the “forces” that are involved with the movement of fluid across the permeable membranes of the capillary beds. Within the capillary, the capillary hydrostatic pressure “forces” fluid out of the capillary and into the interstitium; the interstitial hydrostatic pressure “forces” fluid to leave the interstitium and enter the capillary; the capillary plasma colloid osmotic pressure (also called plasma oncotic pressure) “draws” fluid into the capillary; and the interstitial fluid colloid osmotic pressure (also called oncotic pressure) “draws” fluid into the interstitium. The net movement of fluid across the capillary membrane is affected by both the magnitude of the imbalance between the hydrostatic and osmotic forces and the permeability of the capillary membrane to water. Kf is known as the permeability coefficient.
Thus the net movement of water across the capillary membrane can be expressed via the equation:
Kf[(HPc-HPif)-(COPc-COPif)]
HPc = Hydrostatic pressure in the capillary
HPif = Hydrostatic pressure of the interstitial fluid
COPc = Colloidal osmotic pressure of the capillary plasma
COPif = Colloidal osmotic pressure of the interstitial fluid
