Routine Complete Blood Count and Biochemistry
While these routine laboratory tests are commonly performed in patients with heart disease or heart failure, findings are non-specific and generally reflect either underlying or concurrent disease, may reflect reduced cardiac output, or may be secondary to cardiac medications. Renal biochemistry and electrolytes are frequently used for monitoring purposes in patients receiving cardiac medications, particularly ACE-inhibitors and diuretics.
The two tables below summarize some potential findings on CBC or biochemistry in patients with various types of heart disease and possible mechanisms.
| CBC Finding | Potential Mechanism(s) | Comments |
|---|---|---|
| Anemia | – anemia of chronic disease – neurohormonal activation from reduced cardiac output – renal dysfunction | – common in human patients with chronic HF and a poor prognostic indicator – present in up to 30% of dogs with advanced MMVD and may similarly indicate poorer prognosis |
| Erythrocytosis | – hypoxemia, due to a right-to-left shunt or pulmonary pathology | – erythrocytosis refers to a true elevation in red blood cell count, and not just a relative increase due to decreased plasma volume like in dehydration |
| Stress leukogram | – chronic corticosteroid stimulation as with any chronic stress | |
| Inflammatory leukogram | – underlying inflammatory or infectious causes as may occur with endocarditis, myocarditis, pericarditis | – overall these etiologies are uncommon |
| Biochemistry Finding | Potential Mechanism(s) | Comments |
|---|---|---|
| Azotemia | – prerenal (reduced renal perfusion, diuretic effect) – renal (renal dysfunction) | – prerenal azotemia common in patients receiving diuretics |
| Increased hepatic enzymes | – hypoxia (ALT) – passive cogestion (ALP, bilirubin) | – may have prognostic value |
| Hyponatremia | – neurohormonal activation from reduced cardiac output – diuretic effect | – associated with poor prognosis in humans with chronic HF |
| Hypokalemia | – diuretic effect – renal dysfunction | – more common in cats than dogs, particularly if hyporexic – may require oral supplementation – may exacerbate risk of tachyarrhythmias |
| Hyperkalemia | – acute renal dysfunction – secondary to combination ACE-inhibitor and mineralocorticoid antagonist therapy – reperfusion injury in cats with thromboembolic disease | – uncommon in domestic species with RAAS antagonists, whereas more common in humans – may precipitate bradyarrhythmias |
| Increased CK | – mild to moderate elevations simply due to venipuncture alone – marked elevations in cats with thromboembolic disease and ischemic myopathy | – CK is NOT useful in detecting cardiac muscle damage in domestic animals |
Cardiac Biomarkers
A biomarker is simply a measurable indicator of physiologic or pathophysiologic processes. Just as ALT and creatinine are circulating biomarkers of liver and kidney disease, respectively, circulating cardiac biomarkers have become of diagnostic interest. The two most widely clinically used cardiac biomarkers are brain natriuretic peptide (BNP) and cardiac troponin-I (cTnI).
How useful are these biomarkers to the clinician? It very much depends on the clinical scenario, the information you already have, and the clinical question being asked! These concepts are really important to keep in mind when contemplating the use of a cardiac biomarker in practice. Like any test, a biomarker isn’t meant to be used in isolation, and it should only be performed if it has the potential to add value to what you already know in your diagnostic evaluation.
Here are some examples of clinical questions where a cardiac biomarker might, in theory, be of use:
- I am concerned about an abnormality I’ve detected on my asymptomatic patient’s cardiovascular physical examination (e.g. heart murmur, arrhythmia). What is the likelihood that my patient has significant cardiac disease?
- What is the likelihood that my patient’s respiratory signs are due to congestive heart failure (as opposed to primary respiratory disease or some other process)?
- My patient has cardiac disease. What is my patient’s prognosis?
- My patient has cardiac disease and is being treated with cardiac medication. Is my patient responding appropriately, or should I be doing more?
There is good evidence in the veterinary literature to support the first two questions, whereas the latter two questions have only begun to be explored. Let’s take a deeper dive below!
Brain Natriuretic Peptide (BNP)
Brain natriuretic peptide (BNP or B-type natriuretic peptide), first isolated in the porcine brain, originates predominantly from ventricular myocardial cells. It is released from cardiomyocytes as a prohormone (proBNP) into circulation in response to myocardial stretch or stress, and is cleaved in circulation into the active hormone (C-BNP) and an inactive fragment (N-terminal proBNP or NT-proBNP).
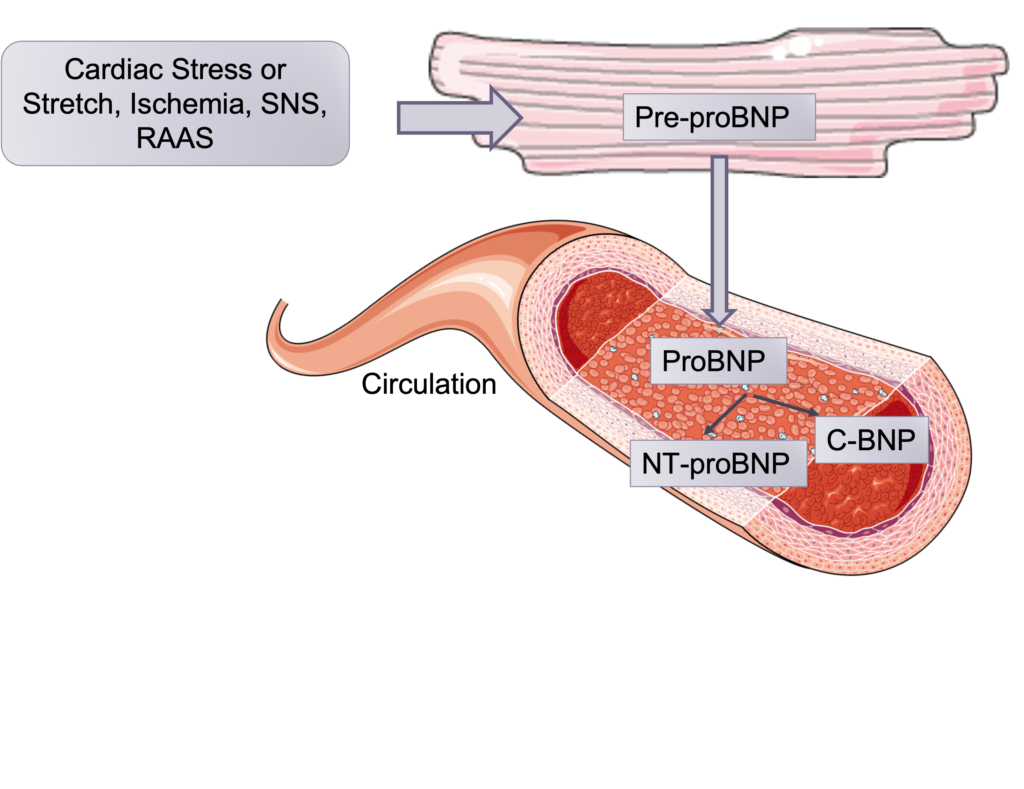
Physiologic actions of the active hormone include natriuresis, diuresis, and vasodilation. The inactive fragment NT-proBNP is more stable and has a longer half-life in circulation and is, therefore, the component quantitated by commercial assays, which are species specific (in North America, Cardiopet® proBNP by IDEXX).
Use of NT-proBNP to detect preclinical disease
Detection of a heart murmur or an arrhythmia in an asymptomatic patient can pose a diagnostic dilemma. When it comes to murmurs, some patients (especially cats) may have physiologic murmurs, are these cannot be reliably distinguished from pathologic murmurs (for instance, due to cardiomyopathy) on auscultation. Furthermore, thoracic radiography lacks sensitivity when it comes to detecting preclinical cardiomyopathy and some other heart diseases in cats and dogs. Echocardiography is the best clinical tool to detect and characterize heart disease, but it is not always readily available to practitioners, and some clients may need additional motivation to pursue this step.
NT-proBNP can be useful to detect moderate to severe structural cardiac disease. It likely won’t detect mild disease, and it is not specific for a particular type of cardiac disease or diagnosis. But it may help provide evidence that the abnormality you are detecting on physical exam (murmur, gallop, arrhythmia) is important and should be pursued with additional diagnostics.
The tables below outline current suggested interpretive criteria for the commercial Cardiopet® proBNP tests in asymptomatic patients:
| FELINE NT-proBNP result | Interpretation |
|---|---|
| < 100 pmol/L OR negative SNAP | clinically significant heart disease is unlikely |
| ≥ 100 pmol/L OR positive SNAP | clinically significant heart disease is likely |
| CANINE NT-proBNP result | Interpretation |
|---|---|
| < 900 pmol/L (< 735 pmol/L in Doberman pinscher) | clinically significant heart disease is unlikely |
| ≥ 900 pmol/L (≥ 735 pmol/L in Doberman pinscher) | clinically significant heart disease is likely |
Use of NT-proBNP to differentiate congestive heart failure from other causes of respiratory distress
- Why might there be a place for this test in cats?
- Many cats with heart disease are asymptomatic
- Radiographic findings in cats with heart disease can be variable and inconclusive
- Heart murmurs or gallops in cats with heart disease may be intermittent, difficult to detect, or not present. Furthermore, innocent or physiologic murmurs are common in cats.
- Although echocardiography is usually definitive, it may not be available or may be expensive
- Role for NT-proBNP in Cats:
- Identify heart disease in high-risk populations that are asymptomatic (to determine if they are “likely” or “unlikely” to have heart disease)
- Older cats
- Cats with either a heart murmur or a gallop
- Breeds at high risk such as the Maine Coon
- Recommendations:
- NT-proBNP > 50 pmol/l is highly likely to indicate underlying heart disease.
- Sensitivity and specificity are reported to be 90% and 85% respectively, however this may apply mostly to the detection of severe disease. Therefore recognize that there is the potential for false negatives, particularly in the case of mild to moderate disease. False positives are also possible.
- For cases that are too fragile for diagnostics or that can’t afford echocardiography.
- Radiographs are always indicated in the presence of respiratory signs, however findings can sometimes be inconclusive.
- Recommendations:
- NT-proBNP > 270 pmol/l is highly likely to indicate the presence of CHF
- Cats with NT-proBNP between 50-270 pmol/l likely have heart disease but may or may not have CHF.
- Identify heart disease in high-risk populations that are asymptomatic (to determine if they are “likely” or “unlikely” to have heart disease)
Use of the NT-proBNP test in Dogs:
- Where might there be a place for this test in dogs?
- To identify dogs with asymptomatic (occult) DCM
- To differentiate between primary respiratory disease and CHF as the cause for respiratory clinical signs
- To assess prognosis and guide therapy
- To identify dogs with asymptomatic heart disease:
- Recommendations:
- NT-proBNP > 900 pmol/l is likely to indicate the presence of heart disease
- Recognize again that both false positives and false negatives will occur.
- Dogs with DCM tend to have higher values than dogs with CMVI
- The more advanced the heart disease the higher the levels of NT-proBNP
- NT-proBNP > 680 pmol/l were associated with radiographic evidence of cardiomegaly (VHS > 11.5)
- Recommendations:
- To differentiate between primary respiratory disease and CHF as the cause for respiratory clinical signs:
- Recommendations:
- NT-proBNP > 2700 pmol/l is highly likely to indicate the presence of CHF in patients with evidence of heart disease.
- Dogs with NT-proBNP between 900-2700 pmol/l likely have heart disease but may or may not have CHF.
- Recommendations:
Limitations:
- Prerenal and renal azotemia may cause significant elevations in NT-proBNP therefore levels must be interpreted with caution in patients with elevated urea and creatinine.
- Pulmonary artery hypertension (without left sided heart disease) also elevates NT-proBNP levels, and may be present in patients with primary respiratory disease.
- Prolonged shipping or inappropriate storage will result in a reduction (degradation) of NT-proBNP.
- Day to day variability likely exists. Week to week variability in normal dogs ranged between 37 to 51%.
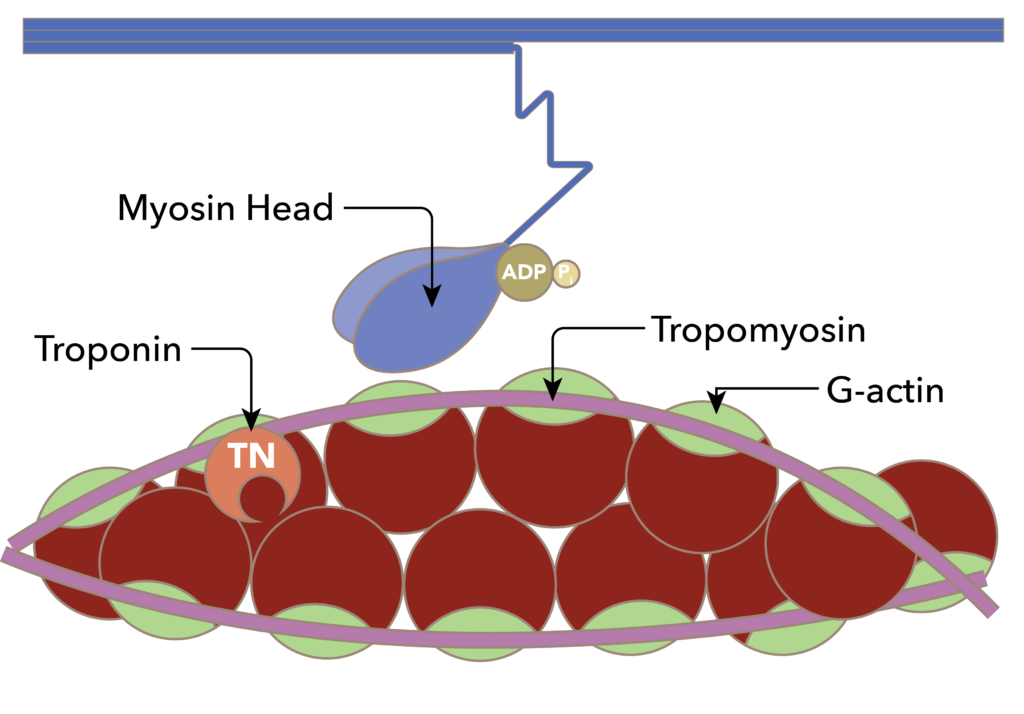
Cardiac Troponin-I (cTnI)
Cardiac troponin-I
Other Specific Laboratory Tests
thyroid, dig levels, coags, blood gas (venous oxygen tension – reduced CO), lactate (reduced CO), amino acid profiles!, serologies (Lyme’s, HW Ag)
